Age alone should not be a barrier to HCT for adults with AML
Research published in Bone Marrow Transplantation concludes that older age in patients with acute myeloid leukemia (AML) should not be a barrier to considering hematopoietic cell transplant (HCT). All age groups (60-64 years, 65-69 years, and 70 years old or older) demonstrated comparable 3-year overall survival (OS) between 40-50%.
This retrospective study of data from the CIBMTR® (Center for International Blood and Marrow Transplantation®) found differences in patient outcomes were associated with factors other than age, such as comorbidities and immunosuppression regimen. This suggests transplant should be considered a standard of care option for patients of all ages who achieve a first complete remission (CR1) instead of considering an upper age limit for HCT eligibility.
Allogeneic HCT is the preferred treatment option for patients diagnosed with AML. However, not all patients achieve CR1, which can be the ideal timing for transplantation. The median age of diagnosis for patients with AML is 67 years, but older patients are not always offered transplant as a treatment option. Reduced-intensity conditioning (RIC) provides the opportunity for older patients with AML to be transplant candidates; however, evidence-based patient selection remains a challenge to broader access.
This study included 1,321 patients with AML 60 years and older who received an allogeneic HCT in CR1 from 2007 through 2017. Patients were split into three categories by age (60-64 years, 65-69 years, and 70 years old or older) with comparable clinical characteristics and comorbidities.
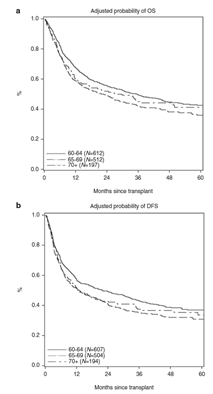
Patients aged 60–64 had better OS, better disease-free survival (DFS), and lower transplant-related mortality (TRM) than the other groups. The 3-year OS for the three cohorts was 49.4% (aged 60-64), 42.3% (aged 65-69), and 44.7% (aged 70 and older), respectively (p = 0.026). Univariate and multivariate analyses were conducted to determine relationships between several variables and any causal factors.
Differences in outcomes were better explained by covariates other than age. Increasing age is associated with a small decrease in OS after transplant, which is smaller than that due to other disease-related risk factors. The impact of increasing age on outcomes showed that all age groups achieved 3-year overall survival of 40-50%. The median follow-up of survivors was nearly 3 years.
According to the research, patient age alone should not represent a hard cut off for transplant consultation, including for patients with AML in CR1. In addition, access to transplantation can improve the overall outcomes for patients with AML, especially when efforts focus on minimizing residual disease and better donor selection. All patients with AML could benefit from early HLA typing at diagnosis, early referral to a transplant center for evaluation, donor identification, optimization of their disease and organ function, and psychosocial support planning to maximize success rates.
Figure 1. Summary of Outcomes for Patients with AML Transplanted in CR1

Maakaron JE, et al., published in Bone Marrow Transplantation