Lack of Strong Relationship between Community Physicians and Transplant Centers Associated with Lower Support for Early Treatment Behaviors and Confidence in Post-Transplant Care
April 2022
According to the research abstract presented at the 2022 Tandem Meetings of the American Society of Transplantation and Cellular Therapy (ASTCT) and the CIBMTR® (Center for International Blood and Marrow Transplant Research®), hematology/oncology physicians with weaker perceived relationships with transplant centers tend to report less support for early treatment behaviors, such as early referral for transplant consultation. In addition, they report less confidence in managing post-transplant care for patients receiving hematopoietic cell transplantation (HCT). Results point to a need for stronger relationships and shared care models to improve patient outcomes and experience when transitioning back and forth between hematology/oncology practices and transplant centers.
Shared care models continue evolving across healthcare, including hematology/oncology practices and transplant centers. Allogeneic HCT provides a unique opportunity for collaboration between physician teams due to the transfer of patients through the phases of transplantation. The objective of this study was to measure the hematologist/oncologist’s perspective of their relationship with regional transplant centers and how it relates to their viewpoints about early treatment and post-transplant care.
Online surveys were given to board-certified United States hematologists and oncologists to measure their relationship strength and treatment perspectives with their local transplant centers. Physicians must have seen at least two patients with acute myeloid leukemia (AML) in a single year within the time frame of the survey.
The survey was conducted from Nov. 24, 2020–Jan. 3, 2021 and included 131 hematologists and oncologists. Pediatric-only physicians, physicians who perform HCT, and those who self-identified as part of a dedicated transplant program within their system were excluded. Relationship strength with transplant centers was measured on a scale of 1 to 7 (1-completely disagree and 7-completely agree) in response to the statement, “I/my practice has a strong relationship with the nearest transplant center(s).” Physicians were then grouped into Strong Relationship (6-7) or Low/Neutral Relationship (1-5) categories.
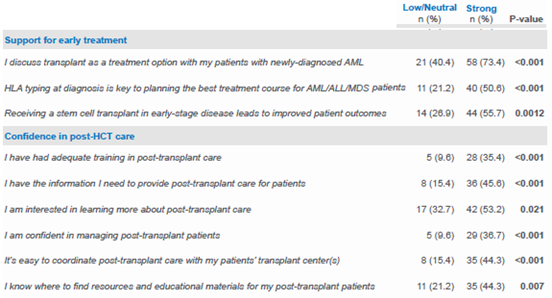
Of the 131 in this study, 52 physicians (39.7%) were in the Low/Neutral group, and 79 (60.3%) were in the Strong group. The Low/Neutral group had a lower agreement with statements supporting early treatment behaviors, such as agreeing that receiving HCT in early-stage disease leads to improved patient outcomes (p=0.0012) (see Table 1). The Low/Neutral group also had a lower agreement with statements indicating confidence in providing post-HCT care, such as agreeing that they have had adequate training in post-HCT care (p < 0.001).
This research reveals that hematology/oncology physicians with a weaker-rated relationship with transplant centers reported less confidence in managing post-transplant care and lower support for early HCT-related treatment interventions. These findings highlight the importance of collaboration between these teams to support a shared care model, which can benefit patients across their transplant journey. Patient outcomes may benefit from a joint physician-team effort to address barriers and plan treatment across the continuum of care.
NMDP is currently partnering with the Dana-Farber Cancer Institute Stem Cell Transplant and Cell Therapy Program to optimize a shared care model to remove barriers to HCT consultation, treatment and post-treatment care, with the goal of expanding treatment options for all patients and improving patient outcomes.
Table 1: Early Treatment and Post-Transplant Perspectives Among Hematology/Oncology Physicians based on Strength of Transplant Center Relationship
Steffens K, Yoo D, Lee T, Sees JA, Lih-Wen M, Tandem poster abstract